Understanding CNS Tuberculomas in Brain Scans
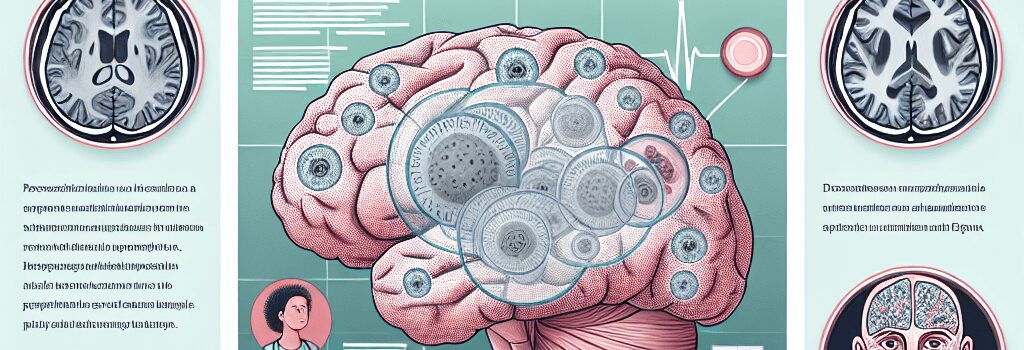
In radiology, the term starry sky conjures images of distant galaxies—but in a clinical emergency department, it describes a radiologic pattern no physician wants to see. In a recent New England Journal of Medicine case report, a 57-year-old South Korean man presented with two weeks of progressive headaches, neck pain, and right-hand tingling. His gadolinium-enhanced MRI revealed innumerable, small, spherical, peripherally enhancing nodules throughout his brain and upper spinal corda manifestation of central nervous system (CNS) tuberculomas.
Clinical Presentation and Diagnostic Challenges
CNS tuberculomas are rare sequelae of Mycobacterium tuberculosis infection. The patients history of pulmonary tuberculosis, previously treated with a standard six-month isoniazid-rifampin regimen, complicated the diagnosis. His cerebrospinal fluid (CSF) analysis was non-revealingacid-fast bacilli smear and PCR were negative. Only a sputum culture returned positive for M. tuberculosis, underscoring the pathogens stealth and the need for multimodal diagnostics.
- Symptom onset: Subacute (1014 days of headache, nuchal rigidity, focal paresthesia)
- Imaging clues: Multiplicity of nodules, perilesional edema, leptomeningeal enhancement
- Laboratory hurdles: Low CSF yield, slow culture turnaround (up to 80 weeks)
Advanced Imaging Modalities and AI-Assisted Analysis
High-field MRI (3 Tesla) with T1-weighted, T2-weighted, FLAIR, diffusion-weighted imaging (DWI), and post-contrast sequences is the gold standard for detecting intracranial tuberculomas. Typical parameters include:
- Slice thickness: 3 mm; TR/TE (T1): 500 ms/15 ms; TR/TE (T2): 4,000 ms/100 ms
- Contrast dose: 0.1 mmol/kg gadobutrol, with 5 min delay for optimal lesion conspicuity
- Advanced sequences: Susceptibility-weighted imaging (SWI) for microcalcifications; DWI for caseous necrosis
Recent advances leverage cloud-based deep learning models (e.g., U-Net architectures) to automate lesion segmentation and volumetric analysis. In a 2024 multicenter trial, AI algorithms achieved 92% sensitivity in detecting tuberculomas >5 mm on T1 post-contrast images, enabling earlier intervention in resource-limited settings via teleradiology.
Pathophysiology and Molecular Mechanisms
Mycobacterium tuberculosis reaches the CNS hematogenously, often protected within macrophages (Trojan horse mechanism). Key steps include:
- Blood–brain barrier traversal: M. tuberculosis exploits endothelial tight junction modulation via ESAT-6 protein.
- Granuloma formation: Aggregates of infected macrophages and T-lymphocytes form caseating masses with central necrosis (caseum).
- Immune evasion: The bacterium secretes protein tyrosine phosphatases (PtpA, PtpB) to suppress intracellular killing.
Calcification within chronic tuberculomas appears as hypointense foci on SWI, reflecting dystrophic mineralization.
Treatment Regimens and Outcomes
The patient underwent an 18-month intensive antimycobacterial regimen, combining isoniazid (5 mg/kg), rifampin (10 mg/kg), pyrazinamide (25 mg/kg), and ethambutol (15 mg/kg) for two months, followed by a continuation phase of isoniazid and rifampin for 16 months. Adjunctive corticosteroids (dexamethasone 0.4 mg/kg/day) reduced perilesional edema and intracranial pressure.
Serial MRIs at 1, 6, and 12 months demonstrated progressive lesion involution; by month 18, imaging was normalized and neurological deficits resolved. The case supports recent WHO 2025 guidelines advocating extended therapy for CNS tuberculosis and monitoring via periodic MRI.
Global Health Implications and Future Directions
Tuberculosis remains the worlds deadliest infectious disease, with 10.6 million new cases and 1.3 million deaths in 2023. A recent phase III trial of the M72/AS01E vaccine showed 50% efficacy in preventing pulmonary TB—yet CNS manifestations underscore the need for advanced diagnostics and therapeutics.
Key future priorities include:
- Point-of-care molecular assays (e.g., CRISPR-based diagnostics) to detect M. tuberculosis DNA in CSF within 2 hours.
- AI-driven telemedicine networks to expand radiology access in low- and middle-income countries.
- Host-directed therapies targeting immunopathology and granuloma resolution.
By combining high-resolution imaging hardware, cloud-based AI pipelines, and novel pharmacotherapies, the medical community aims to turn the ominous starry sky into a constellation of preventable and treatable nodules.